Let's Not Panic About Training In A Pandemic!

Sandra Speller.
Physiotherapist and Professional Head of Therapies
Sussex Community NHS Foundation Trust
The role of community trusts at the height of the pandemic is perhaps a little under-appreciated, but this is probably understandable, given the high numbers of critically ill patients of all ages requiring intensive and complex healthcare at the time. We all watched the news each night as the crisis unfolded, and saw the numbers of patients being prone nursed, supported with CPAP - and for those most affected, ventilated as their lungs became unable to draw in enough oxygen to sustain life without mechanical help. We saw patients managed in ITUs, in operating theatres and in every nook and cranny in some acute hospitals, all requiring high level care. Releasing capacity to allow this space to be found meant moving other patients out – that phrase we all dread, particularly during winter pressures, of "maintaining patient flow" became the most important task across health and social care systems, driven nationally.
Ensuring we had the capacity to manage the expected patient numbers, and increased complexity of need meant stopping or significantly reducing much community provision, including MSK, podiatry, child development services and work by specialist teams such as community neurology and falls services. This allowed many AHP staff to be redeployed to support both our community hospital wards and community therapy provision - and ultimately maintain that absolutely essential movement of patients out of acute care. There have been many plaudits for the NHS on how it coped at the height of the pandemic, with no reports of overwhelmed hospitals, no reports of the sort of challenges faced by our counterparts in Italy – and we in community services can be very proud of the part we played in this response. Community hospitals were very important cogs in the NHS machine, without which the news reports may have looked very different.
So …. we had a supply of additional staff to support this increased and fast paced patient flow from acute to community – but how did we make sure they were able to be effective, safe and confident clinicians in what was, for many, a very different field of work? We had paediatric OTs who had not worked with anyone over the age of eighteen for 30 years, and MSK physios who were more used to managing complex spinal pain and rehabbing people back to county level sport - all suddenly expected to assess, treat and provide equipment to get the usual community hospital cohort of elderly, frail patients with complex co-morbidities home or into appropriate care placements. Training and skilling up such a diverse workforce at speed, to manage the therapy requirements for these patients was obviously a challenge – particularly in a large community trust, with a large number of community beds, spread over a large geographical area.
What we did
The key important first step was identifying the essential skills that were needed, and asking those staff who were being redeployed to self-assess their current level of knowledge, competency and confidence with the skills identified – which included medical (recognising the deteriorating patient, taking basic observations), care (support with washing, dressing , toileting, eating and drinking and patient handling) as well as therapy tasks – which may have been rusty, but not fully forgotten!
Luckily we have recently developed clinical skills facilitator roles for our adult therapy teams; these staff are responsible for the training of our unregistered therapy workforce and supporting their competency development and sign off out in clinical practice. At the end of 2019 they had developed and delivered an extremely successful 3-day training programme for recently employed band 3 therapy assistants, receiving fantastic feedback. This training covered many basic therapy skills – mobility aids, managing stairs, strengthening and balance exercises, dressing and kitchen assessments and home equipment provision.
Helpfully these were exactly the therapy skills we were going to need quickly on our units, so it made absolute sense to use the expertise of our clinical skills facilitators to develop and deliver what was needed – and how fabulously did they rise to the challenge! I also pulled in one of our respiratory physiotherapists to develop a quick resource on Covid-19 and its impact, and some key advice on managing breathlessness. Together with the nursing practice development team and members of the project management team (who were redeployed to help) we commandeered the largest space in the Trust as our "Training HQ". The plan was to develop training videos and run interactive training and Q&A sessions from here, which we did over a period of about 4 weeks – with so much to plan and deliver it certainly needed military style organisation to co-ordinate and manage!
How did we do it?
Deciding which video resources would be helpful to support staff was the easy part! How did we get over 26 videos made quickly, the content reviewed and checked for assurance and ready for staff consumption in about a week? Cue our knight in shining armour, the man who had an answer or solution for every question or problem, and certainly didn't like to be beaten – our Digital Lead, who was a fantastic support with every stage of the process – and even didn't mind being called via What's App when he was out walking his dogs on a very blustery South Downs! After a couple of false starts we used a simple tablet set up – propped on a range of boxes and files to get the right height and angle. What we got was certainly not Oscar quality, but the videos were clear, with good sound quality and absolutely met the brief: quick, simple, bite size video clips demonstrating "how to" … walk a patient/ help them out of a chair/help a patient eat/get washed/get dressed/assess for walking frame/ hoist from chair to bed/ complete standing transfer etc; etc;
Our clinical skills facilitators became very adept at film direction and editing as they went, and by the 15th video were running through smoothly with minimal rehearsal and a good turn in ad-libbing! The videos were then reviewed for clinical content by senior clinicians, the AHP Lead and Chief Nurse and "editorial quality" (a couple got rejected for sound quality early on by the Digital Lead!) and uploaded very quickly onto an internal YouTube® platform. We developed a dedicated "Covid training" page on our intranet, which meant staff could access "any time, any place, anywhere" - and as we had broken down topics into bite sized pieces it made it much easier for staff to personalise their learning and updates – nothing worse than sitting through a whole 45 minute lecture or training package for the one small item you need!
Staff appetite for, and engagement with the videos was excellent; we monitored levels of uptake, which in turn helped us see in which areas staff were seeking support. For example, we had 431 views on slings and sling insertion, 260 on how to support sit to stand with a stand aid, 345 on toileting, 298 on washing and dressing, 204 on mobilising with a frame, 165 on techniques for managing breathlessness and 98 on basic home equipment.
We also sought feedback from staff when they had completed their learning to make sure we were meeting the needs of all the staff being redeployed, who were coming from a huge range of differing professions and years of experience. The staff reaction suggests the approach taken was more than adequate, as the feedback was very positive, with comments such as "I have seen the videos. Very Informative and helpful" and "feel much more confident to go back to the "adult world" now!"
The impact on staff confidence of using this approach is best explained by this health visitor:
"I just wanted to say thank you for taking the time & effort to put together the YouTube clips, especially the basic care clips. I am a health visitor about to be deployed to the adult rehab unit at ZM Hospital. I am an adult trained nurse but It's been almost 22 years since I last worked in a ward environment so I've found these really helpful. I'm going to be redeployed as an HCA for this reason. One of the reasons I left the acute environment was because I felt I didn't have the time to spend doing 'basic care' (I worked on CCU, emergency medical admissions units). Now I've watched these videos I am really looking forward to spending some time with patients, chatting & helping them with their activities of living & am no longer panicking about which way elbows bend!"
For many staff a quick view of a video was enough to reassure that the knowledge needed was still there; however, we also recognised that for some of our redeployed staff – such as our speech and language therapists and podiatrists, helping patients to wash, dress and use the toilet was not in their basic professional training, so would all be new skills, and they would have questions and concerns that a video alone would not be able to answer. Therefore, for a period of 4 weeks we set up camp in our large manual handling training room and ran a daily programme of interactive Skype sessions on:
- Patient handling – using patient handling equipment
- Assisting with basic care
- Supporting mobility
- Respiratory management
This was done on a rolling rota, so different sessions were available at different times each day; this provided staff flexibility to fit in with their working and home lives, as we have many part-time staff. These sessions enabled staff to ask questions on anything they were not sure about after watching the video resources, or to ask the clinical skills facilitators to demonstrate a technique again. They also called on the help of some of our wonderful therapy practitioners and assistants to support and answer questions, which in turn was a great development opportunity for them! At this point different technical skills were called upon – we all got quite good at following the clinical skills facilitators running the session around with a laptop as they leapt up to demonstrate a certain technique on request, moving forwards and closer to zoom in close as required! Again, the feedback was great for these sessions, with staff really valuing the calm expertise from our staff, and the opportunity to learn directly from those who were doing such tasks on a daily basis. The patient handling equipment sessions were particularly popular, with over 140 staff joining at least one session (some staff did come back for more!) We found that as staff started to go out in their new roles they would often "dial in" for help with specific situations they had come across. Again, the staff feedback shows how much these sessions were important to staff confidence - "all your sessions have been really helpful.... wish you were all coming with us on deployment!!!!! Thank you so much"
What we have learnt?
- You can produce suitable quality video resources with basic equipment – in fact the patient handling equipment videos now form part of our Trust's mandatory patient handling training
- Staff found video refreshers very helpful, and for many staff were enough to give them the confidence to get out in a very different area of healthcare and support patient care delivery
- Interactive sessions and the opportunity to ask questions can be a very helpful addition to increase staff confidence
- The positive feedback on the training during this period has meant we have taken the same approach to our new band 4 therapy training package - which is being run as we speak, as we continue to need to live as far as possible in the virtual world! This is going well so far, and has made it easier to release staff to join the training. Watch this space.






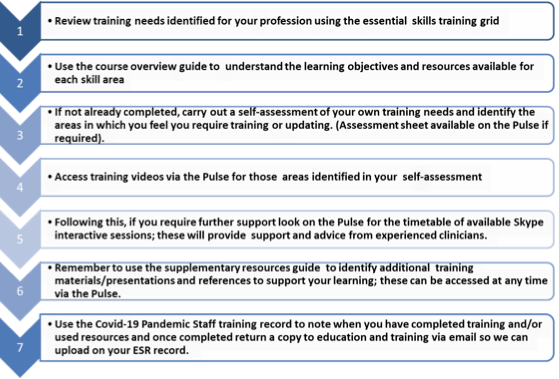
Summary Of Training Process - Instructions For Staff